
Divya Bhatia
Tagline:Advancing Science Through Innovation
New York, NY, USA
BIO
Highly organized, results-driven, and forward-thinking immunologist, holds a PhD, and 9 years of academic experience in translating immunology research into actionable insights and innovative solutions.
👩🏻🔬 Proven ability to lead independent research, drive collaborative projects, mentor trainees, and work across disciplines to design and solve complex biological questions.
🔬 Successfully led projects uncovering immune and mitochondrial functions of myeloid cells, intercellular, and interorgan communication that earned national recognition for scientific innovation and consistently selected for oral presentations.
🧫 Demonstrated proficiency in preclinical disease models, immune cell isolation, activation, expansion, modification, adoptive transfer, and analysis using multiple strategies.
💰 Secured competitive funding as Principal Investigator, validated scientific independence.
📝 Authored 23 manuscripts (12 as a first author), edited two books, and presented research globally (>12 oral, >30 abstracts), demonstrating expertise in communicating science.
💊 Passionate about leveraging her immunology background, technical expertise, and analytical mindset to drive innovation in therapeutic discovery.
LINKS.
https://vivo.weill.cornell.edu/display/cwid-dib2020
https://loop.frontiersin.org/people/574232/overview
https://orcid.org/0000-0002-8236-3440
Talk:
EXPERIENCE
Instructor of Immunology
from: 2022, until: presentField of study:ImmunologySchool:Weill Cornell MedicineLocation:New York, USA
Description► Independently designed, executed, and led three research projects focused on functions of macrophages during kidney and lung inflammation, and fibrosis. The work involved isolating, differentiating, activating, and engineering macrophages. Published 15 peer-reviewed manuscripts, including a) Bhatia D. et al., JCI Insight 2019; and b) Bhatia D. et al., Kidney Int. 2022.
► Established and maintained interdepartmental and interinstitutional collaborations leading to publications, including: a) Chung KP, Hsu CL, Fan LC, Huang Z, Bhatia D, et al., Nat Commun. 2019; b) Patino E, Bhatia D, et al., JCI Insight. 2023; and c) Kallinos E, Chung KP, Torres LK, Bhatia D, et al., Am J Physiol Lung Cell Mol Physiol. 2025.
► Provided training in surgical models, adoptive transfer of drug (iron)-treated macrophages, and quantitative data analysis, with a focus on dose- and route-dependent effects of the drug (iron).Postdoctoral Associate
from: 2016, until: 2022Field of study:ImmunologySchool:Weill Cornell MedicineLocation:New York, USA
Description► Designed projects investigating the functions of myeloid cells in the progression of kidney fibrosis, utilizing mouse models and human specimens. Performed isolation, activation, and culture of PBMCs, BMDM, and other primary cells from tissue.
► Presented findings to establish and strengthen collaborative research projects.
► Trained Research Associates and Visiting Fellows in advanced experimental techniques, including cytometric bead array, multicolor flow cytometry, using Fortessa, LSR II, Canto, Symphony, Accuri C6, data analysis using FlowJo and GraphPad Prism, blood/tissue harvesting, IP/SC injections, primary cell isolations, cell co-culture (direct and indirect), transfection, western blotting, confocal microscopy, and ELISA.Visiting Research Fellow
from: 2014, until: 2014Field of study:ImmunologySchool:University of BristolLocation:Bristol, UK
Description► Standardized assays for evaluating the effects of Th17 cell-derived IL-17, human plasma, and PBMCs from patients with relapse or remission of nephrotic syndrome on podocytes’ cytoskeletal stability.
► Built a strong rapport with the scientific group through active discussions in the group meetings.Senior Research Fellow
from: 2011, until: 2016Field of study:ImmunologySchool:All India Institute of Medical SciencesLocation:New Delhi, India
Description► Designed and executed projects investigating the efficacy of different drugs on functional responses of Th1, Th2, Th17, T regulatory cells, naive, memory, and regulatory B cells. Studied the effects of rituximab in patients with nephrotic syndrome under a trial approved by the Drugs Controller General of India. The findings from the project entitled “Rituximab modulates T- and B-lymphocyte subsets and urinary CD80 excretion in patients with steroid-dependent nephrotic syndrome”, Bhatia et al., Pediatr Res., 2018, were featured on journal’s cover. Contributed to a randomized clinical trial comparing how mycophenolate mofetil and levamisole impact T and B cell biology in frequently relapsing nephrotic syndrome patients.
► Provided training in PBMCs isolation, culture, and standardized surface and intracellular staining for T and B lymphocyte markers.
► Published seven peer-reviewed papers and presented over 10 abstracts, including an oral presentation at the International Pediatric Nephrology Association’s 2016 meeting in Brazil.
► Prepared and submitted annual reports for two different research projects annually to the British Council and the Indian Council for Medical Research. Coordinated between the All India Institute of Medical Sciences, New Delhi, the University of Bristol, UK, and the University of Michigan, USA as part of a trilateral collaborative project on nephrotic syndrome by presenting updated research findings.
► Established a cell culture facility and developed biobanking protocols to ensure reproducible sample processing and analysis.Research Assistant
from: 2009, until: 2011Field of study:Cell BiologySchool:JR Kisan Homoeopathic Medical College & HospitalLocation:Haryana, India
Description► Recorded data and maintained source documentation.
► Guided undergraduates in completing their lab assignments.
► Stocked, organized lab supplies, and managed lab operations.Class Representative (Elected), Bachelor of Science Program
from: 2004, until: 2006Field of study:LeadershipSchool:MD UniversityLocation:Haryana, India
Description► Elected as a Class Representative (CR) at the college level for two consecutive years to represent a cohort of 60+ students.
► Served as the primary liaison between students and the College Principal and faculty, communicating academic and administrative concerns.
► Organized visiting lectures and academic activities to enhance student learning and engagement.
► Contributed to curriculum feedback and initiatives aimed at improving course structure throughout a two-year tenure.
► Selected for the “Miss Final” Award in the final year, an honor awarded to one student per graduating class in recognition of overall excellence and leadership.
EDUCATION
- PhD (Immunology) All India Institute of Medical Sciences, New Delhi, India (2011-2017): Thesis paper featured on the journal's cover, see publication.
- MPhil (Biotechnology) Vinayaka Missions Research Foundation, Tamil Nadu, India (2008-2009).
- MS (Medical Biotechnology) Maharshi Dayanand University, Haryana, India (2006-2008).
- BS (Life Sciences) Maharshi Dayanand University, Haryana, India (2003-2006).
HONORS AND AWARDS
2025. George M. O'Brien Kidney Resource Alliance (OKRA) Opportunity Pool Program Award, The University of Alabama at Birmingham, AL.
2025. Science and Innovation Working Group Award, Allergy, Immunology and Inflammation (AII) Assembly, American Thoracic Society, NY.
Science and Innovation Working Group Award, Allergy, Immunology and Inflammation (AII) Assembly, American Thoracic Society 2025. Abstract Scholarship, American Thoracic Society, NY.
Abstract Scholarship, ATS 2023. Research profile published in the American Journal of Physiology-Renal Physiology (https://journals.physiology.org/doi/full/10.1152/ajprenal.2023.325.1.AU).
2022, 2024. Judge, Vincent du Vigneaud Memorial Research Symposium, Weill Cornell Medicine, NY.
2022. T32 NIH Ruth L. Kirschstein National Research Service Award (NRSA), NY.
2022-2023. Judge, Medical Student Research Day, Weill Cornell Medicine, NY.
2021-2022. Judge, NSPC Health Science Competition, Center for Science Teaching & Learning, NY.
2016. Travel grant, International Pediatric Nephrology Association (IPNA), Brazil.
2014. Postgraduate Research Scholarship, University of Bristol, United Kingdom.
2013-2015. Fellowship, UK-India Education & Research Initiative, British Council, India.
2012. PhD and Journal Club Representative, Department of Pediatrics, AIIMS, India.
2011-2013. Fellowship, Indian Council of Medical Research (ICMR), India.
2010. National Eligibility Test, Council of Scientific & Industrial Research (CSIR), Ministry of Science and Technology, India.
2006. “Ms. Final”, Government College for Women (awarded to one student per graduating class).
2004-2005. Class Representative, elected for two years in a row, Government College for Women, India.
INVITATIONS TO SPEAK/ORAL PRESENTATION
Regional*
2025. Kidney-Lung Communication: Mitochondrial Fusion Proteins Modulate Alveolar Macrophage-Epithelial Cell Interaction. The Briscoe-King Lung Club, New York.
2025. Kidney-Lung Communication: How Mitofusins Regulate Lung Macrophage-AEC2 Crosstalk During Kidney Fibrosis-associated Lung Injury. Pulmonary Basic & Translational Research Conference, New York.
2023. Lung-Kidney Crosstalk: Interrogating Myeloid and Alveolar Epithelial Type 2 Cell-specific Functions of Mitofusins During Kidney Fibrosis-associated Lung Injury. Pulmonary Basic & Translational Research Conference, New York.
2019. Transgenic Mouse Models in Biomedical Research. Postdoc Pub Talk, Weill Cornell Medicine, New York.
2019. Role of Macrophage Mitophagy During Kidney Fibrosis. Postdoc Research Day, Weill Cornell Medicine, New York.
2018. Macrophage Mitophagy Protects Against Kidney Fibrosis. The Rogosin Institute, New York.
2017. Role of Macrophage Mitophagy Against Kidney Fibrosis. 2nd Annual Weill Department of Medicine Research Retreat, New York.
National*
2025. Mitochondrial Fusion Protein-mediated Interaction Between Lung Macrophages and Type 2 Alveolar Epithelial Cells Prevents Lung Injury and Deleterious Kidney-lung Crosstalk. American Thoracic Society Conference, San Francisco.
2023. Macrophage Mitochondrial Functions: Implications for Experimental and Human CKD. Division of Nephrology, University of Oklahoma Health Sciences Center, Oklahoma (Virtually).
2019. Macrophage Mitophagy Deficiency Promotes Experimental and Human Kidney Fibrosis. American Society of Nephrology Kidney Week, American Society of Nephrology, Washington, DC.
2018. PINK1-MFN2-Parkin-Mediated Mitophagy Dependent Macrophage Reprogramming Protects Against Renal Fibrosis. American Society of Nephrology Kidney Week, San Diego.
2017. Macrophage Mitophagy Modulates Pro-fibrotic Response in Renal Fibrosis. American Society of Nephrology Kidney Week, New Orleans.
International*
2015. Rituximab Modulates T & B-cell Subsets and Urinary CD80 (uCD80) Excretion in Patients with Steroid-Dependent Nephrotic Syndrome (SDNS). Congress of the International Pediatric Nephrology Association (IPNA), Paraná (Brazil).
2015. Incomplete Penetrance of CD46 Mutation Causing Familial Atypical Hemolytic Uremic Syndrome. CEFIPRA Indo-French Collaboration, Joint meeting, New Delhi (India).
2014. Updates: Research on Nephrotic Syndrome. UK-India Education and Research Initiative joint meeting, New Delhi (India).
*Entries categorized based on current geographic location.
GRANT SUPPORT
Role: Principal Investigator (Sub-award).
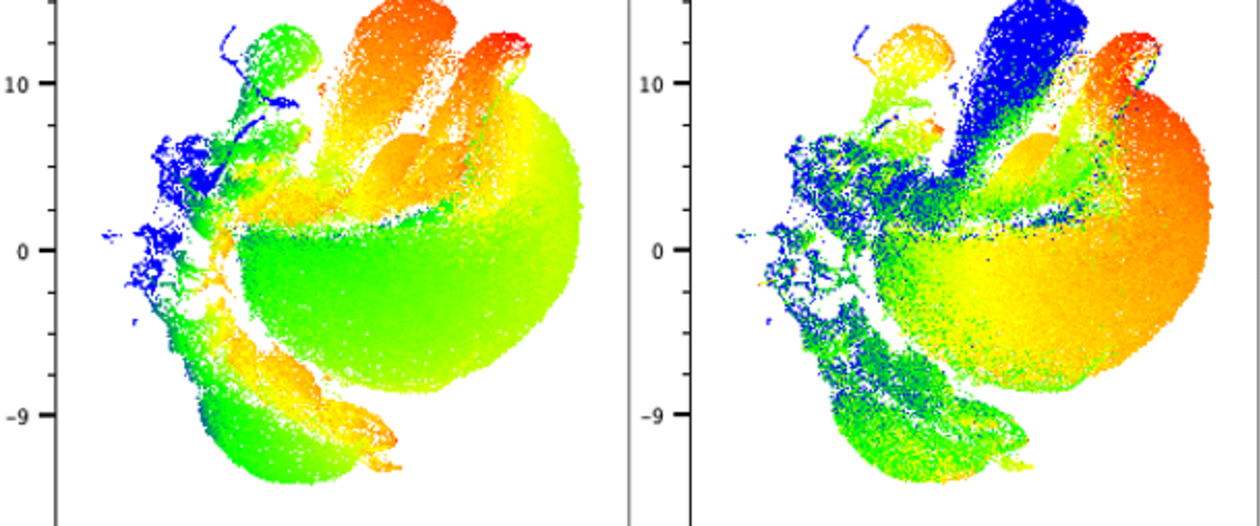
Title: Mitofusins Modulate Kidney Fibrosis-associated Lung Injury and Kidney-Lung Deleterious Crosstalk.
5U24DK137318, University of Alabama (NIH/NIDDK), 07/01/2025-06/30/2026.
The goal of this George M. O'Brien Kidney Resource Alliance (OKRA) Opportunity Pool Program sub-award is to provide a fundamental understanding of the mechanisms of CKD-associated lung injury and its impact on the progression of kidney fibrosis.
Role: Co-Investigator.
Title: Distinct and Overlapping Pathways of Fibrosis and Emphysema in Cigarette Smokers.
5P01HL114501-09, NIH/NHLBI, 07/01/2025-04/30/2026.
This program project grant integrated the expertise of investigators from COPD and IPF communities, both basic and translational/clinical researchers, to come together to better understand the pathogenesis of these chronic lung diseases, and hopefully identify new molecular targets in the treatment of these dreadful diseases in the future.
Role: National Research Service Award (T32) Fellow.
Title: Multidisciplinary Approach Training in Respiratory Research.
T32 HL134629, NIH/NHLBI, 07/01/2022- 06/30/2025.
This training grant supports some of the most promising trainees for up to 3 years. The main objective of this program is to provide a structured, intensive research experience and multidisciplinary mentoring that fosters the development of skills needed to pursue a successful career in investigative pulmonary sciences. My project aimed to elucidate mechanisms of CKD-associated lung injury.
Role: Postdoctoral Associate.
Title: Novel role of RIPK3-dependent necroptosis pathway in lung and kidney fibrosis.
R01 HL133801, NIH/NHLBI, 08/01/2017- 07/31/2021.
This project focused on investigating the functions of RIPK3, MLKL, and fatty acid synthesis pathways in experimental models of lung and kidney fibrosis. My role was to investigate the functions of macrophages in the progression of kidney fibrosis.
Role: Doctoral Scholar.
Title: Research on Nephrotic Syndrome.
UKIERI-TRP-2012/13-001, British Council, 08/13/2013 – 12/22/2015.
This trilateral collaborative project focused on studying the impacts of Th17 cell-derived cytokines on podocyte cytoskeleton and motility.
Role: Visiting Research Fellow.
Title: Th17 cells and Podocyte Crosstalk.
1355468, Renal Academic Unit, University of Bristol 6/16/2014 - 09/13/2014.
Investigated the effects of plasma from patients in relapse versus remission of nephrotic syndrome, and Th17 cell–derived IL-17 on the migratory functions of human podocytes.
Role: Senior Research Fellow.
Title: Effects of rituximab on lymphocyte subsets in children with difficult nephrotic syndrome.
5/4/7-12/1-NCD-II, Indian Council of Medical Research. 09/03/2011 – 08/12/2013.
Aimed to compare lymphocyte subsets in patients with and without response to rituximab during a 1-year follow-up. Focused on B cells (naïve, memory) and T cells (cytotoxic, helper [Th1, Th2], activated, naïve, memory, regulatory), measured at baseline, 1 month, and 1 year post-treatment or at first relapse.
CERTIFICATIONS
Culturing Kidney Organoids: Best Practices for Differentiation and Long-Term Maintenance. Proteintech. 09/23/2025.
Forward Program. McKinsey & Company, 04/24/2025 – 07/07/2025.
Biomedical Research Investigators and Key Personnel. CITI Program, NY, 05/01/2025.
Spectral Flow Cytometry. Memorial Sloan Kettering Cancer Center, NY, and International Society for Advancement of Cytometry, 01/27/2025 - 01/31/2025.
Responsible Conduct of Research. Memorial Sloan Kettering Cancer Center, NY, 01/24/2024 - 03/20/2024.
Practical Genomics. Johns Hopkins University, Maryland and Weill Cornell Medicine, NY, 10/30/2023 - 10/31/2023.
Planning & Writing Successful Grant Proposals. Clinical and Translational Science Center. Weill Cornell Medicine, NY, 06/23/2023.
Chip-Based Cell Sorting. Weill Cornell Medicine, NY, 02/02/2024.
MetaR Tables to Heatmap Generation. Clinical and Translational Science Center, Weill Cornell Medicine, NY, 02/11/2020.
Launching Undergraduate Science Teaching Careers. The Rockefeller University, NY, 10/19/2019 - 12/03/2019.
Research Compliance: Grants & Contracts. Health Care Compliance Strategies (HCCS), NY, 11/09/2016.
Rodent Surgery. Memorial Sloan Kettering Cancer Center, NY, 10/02/2016.
C14 Certified for Supervising Non-production Chemical Laboratories. New York City Fire Department, NY, 10/15/2016.
Workshop on Flow Cytometry Data Analysis. Flow Cytometry Solutions Private Limited, New Delhi, 08/30/2013 - 08/31/2013.
BD Accuri C6 Personal Flow Cytometer Training Course. BD Biosciences, New Delhi, 05/17/2012.
National Training Program in Electron Microscopy for Scientific Investigators. All India Institute of Medical Sciences, New Delhi, 11/14/2011 - 11/26/2011.
V3 Western Blot Work Flow Workshop. Bio-Rad Laboratories, New Delhi, 12/19/2011 - 12/20/2011.
Digital Flow Cytometry. BD Biosciences, New Delhi, 05/23/2011 - 05/25/2011.
Bioinformatics Course. ZAD Institute of IT & Management, Haryana. 09/01/2008 - 08/31/2009.
Training in Microbiology. All India Institute of Medical Sciences, New Delhi, 04/01/2008 - 06/30/2008.
DNA-Based Diagnostics Workshop. Department of Animal Biotechnology, Haryana Agricultural University, Haryana. 11/13/2007 - 12/04/2007.
EDITORIAL BOARD MEMBERSHIPS AND PEER REVIEW
Editorial Responsibilities.
2025-present. Review Editor, Frontiers in Immunology (Inflammation).
2023-present. Review Editor, Frontiers in Pharmacology (Renal Pharmacology).
2022-present. Guest Editor, Frontiers in Pharmacology.
2021-2022. Topic and Review Editor, Cells.
Ad hoc Peer Reviewer for the following Journals.
Journal ad hoc reviewing: 80+ manuscripts.
Journal editing: 12 manuscripts
Cell Press, American Journal of Physiology-Cell Physiology, Scientific Reports, The Federation of American Societies for Experimental Biology (FASEB), The Journal of Clinical Investigation, American Journal of Nephrology, Frontiers in Medicine (Nephrology), Frontiers in Cell and Developmental Biology, Frontiers in Pharmacology (Renal Pharmacology), Frontiers in Endocrinology, Cells, Aging, Journal of Cellular and Molecular Medicine, PeerJ, Diabetes, Metabolic Syndrome and Obesity, Karger Publisher, Pediatric Research, Pediatric Reports, Renal failure, Oncotarget
Guest editor: The following two books were edited as a guest editor.
https://www.google.com/books/edition/Diabetic_Kidney_Disease_Routes_to_drug_d/3QHWEAAAQBAJ?hl=en
PUBLICATIONS
Small but mighty: Hypoxia-responsive tRNA-derived small RNA as a novel regulator of RNA autophagy and kidney protection
Journal ArticlePublisher:Kidney InternationalDate:2025Authors:Divya BhatiaMary E. ChoiHigh fat diet obesity exacerbates acute lung injury induced dysregulation of fatty acid oxidation in alveolar epithelial type 2 cells.
Journal ArticlePublisher:American Journal of Physiology Lung Cellular and Molecular PhysiologyDate:2025Authors:E. KallinosKuei-Pin ChungLisa K TorresD. BhatiaBaran ErsoyP. CarmelietWilliam ZhangHeather W. Stout-DelgadoA. M. ChoiM. PlatakiEditorial: Diabetic kidney disease: routes to drug development, pharmacology and underlying molecular mechanisms, volume II
Journal ArticlePublisher:Frontiers in PharmacologyDate:2025Authors:Divya BhatiaS. SrivastavaEditorial: Diabetic kidney disease: routes to drug development, pharmacology and underlying molecular mechanisms
Journal ArticlePublisher:Frontiers in PharmacologyDate:2023Authors:Divya BhatiaS. SrivastavaAutophagy and mitophagy: physiological implications in kidney inflammation and diseases.
ReviewPublisher:American Journal of Physiology Renal PhysiologyDate:2023Authors:D. BhatiaMary E. ChoiIron therapy mitigates chronic kidney disease progression by regulating intracellular iron status of kidney macrophages
Journal ArticlePublisher:JCI InsightDate:2022Authors:E. PatiñoD. BhatiaS. VanceA. AntypiukR. UniChantalle A. CampbellCarlo G. CastilloShahd JaouniF. VinchiMary E. ChoiOleh M. AkchurinConditional deletion of myeloid-specific mitofusin 2 but not mitofusin 1 promotes kidney fibrosis.
Journal ArticlePublisher:Kidney internationalDate:2022Authors:D. BhatiaAllyson CapiliK. NakahiraT. MuthukumarL. TorresA. ChoiMary E. ChoiAutophagy in kidney disease: Advances and therapeutic potential.
Journal ArticlePublisher:Progress in molecular biology and translational scienceDate:2020Authors:D. BhatiaMary E. ChoiMitochondrial dysfunction in kidney injury, inflammation, and disease: potential therapeutic approaches
ReviewPublisher:Kidney Research and Clinical PracticeDate:2020Authors:D. BhatiaAllyson CapiliMary E. ChoiCarbonyl iron and iron dextran therapies cause adverse effects on bone health in juveniles with chronic kidney disease.
Journal ArticlePublisher:Kidney internationalDate:2020Authors:E. PatiñoS. DotyD. BhatiaKelly MezaYuan-Shan ZhuS. RivellaMary E. ChoiOleh M. AkchurinC-Terminal Fibroblast Growth Factor-23 Levels in Non-Nutritional Hypophosphatemic Rickets
Journal ArticlePublisher:The Indian Journal of PediatricsDate:2019Authors:Joyita BharatiD. BhatiaP. KhandelwalN. GuptaA. SinhaR. KhadgawatP. HariA. BaggaMitofusins regulate lipid metabolism to mediate the development of lung fibrosis
Journal ArticlePublisher:Nature CommunicationsDate:2019Authors:Kuei-Pin ChungChia-Lang HsuLichao FanZiling HuangD. BhatiaYi-Jung ChenS. HisataS. ChoK. NakahiraM. ImamuraMary E. ChoiChong-Jen YuS. CloonanA. ChoiMitophagy dependent macrophage reprogramming protects against kidney fibrosis.
Journal ArticlePublisher:JCI insightDate:2019Authors:D. BhatiaKuei-Pin ChungK. NakahiraE. PatiñoM. RiceL. TorresT. MuthukumarA. ChoiOleh M. AkchurinMary E. ChoiThe Emerging Role of Mitophagy in Kidney Diseases.
Journal ArticlePublisher:Journal of life sciencesDate:2019Authors:D. BhatiaMary E. ChoiBeclin-1 regulates cigarette smoke-induced kidney injury in a murine model of chronic obstructive pulmonary disease.
Journal ArticlePublisher:JCI insightDate:2018Authors:M. PabonE. PatiñoD. BhatiaJocelyn QuinteroKevin C. MaE. FinkelszteinJ. C. OsorioFaryal MalickF. PolverinoC. OwenS. RyterA. ChoiS. CloonanMary E. ChoiInterleukin-6 Contributes to the Development of Anemia in Juvenile CKD
Journal ArticlePublisher:Kidney International ReportsDate:2018Authors:Oleh M. AkchurinE. PatiñoVidhi DalalKelly MezaD. BhatiaSimon BrovenderYuan-Shan ZhuS. Cunningham‐RundlesE. PerelsteinJuhi KumarS. RivellaMary E. ChoiRituximab modulates T- and B-lymphocyte subsets and urinary CD80 excretion in patients with steroid-dependent nephrotic syndrome
Journal ArticlePublisher:Pediatric ResearchDate:2018Authors:D. BhatiaA. SinhaP. HariShailaja SoporyS. SainiMamta PuraswaniHimanshi SainiD. MitraA. BaggaMutations in membrane cofactor protein (CD46) gene in Indian children with hemolytic uremic syndrome
Journal ArticlePublisher:Clinical Kidney JournalDate:2017Authors:P. KhandelwalS. BirlaD. BhatiaMamta PuraswaniHimanshi SainiA. SinhaP. HariArundhati SharmaA. BaggaEfficacy and safety of rituximab in children with difficult-to-treat nephrotic syndrome.
Journal ArticlePublisher:Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal AssociationDate:2015Authors:A. SinhaD. BhatiaA. GulatiM. RawatA. DindaP. HariA. BaggaIncomplete penetrance of CD46 mutation causing familial atypical hemolytic uremic syndrome
Journal ArticlePublisher:Pediatric NephrologyDate:2015Authors:D. BhatiaP. KhandelwalA. SinhaP. HariH. CheongA. BaggaSerum-soluble urokinase receptor levels do not distinguish focal segmental glomerulosclerosis from other causes of nephrotic syndrome in children.
Journal ArticlePublisher:Kidney internationalDate:2014Authors:A. SinhaJ. BajpaiS. SainiD. BhatiaAarti GuptaMamta PuraswaniA. DindaS. AgarwalShailaja SoporyR. PandeyP. HariA. BaggaPrompt plasma exchanges and immunosuppressive treatment improves the outcomes of anti-factor H autoantibody-associated hemolytic uremic syndrome in children.
Journal ArticlePublisher:Kidney internationalDate:2014Authors:A. SinhaA. GulatiS. SainiC. BlancAarti GuptaB. GurjarHimanshi SainiShambhuprasad T KotreshU. AliD. BhatiaA. OhriManish KumarI. AgarwalS. GulatiK. AnandM. VijayakumarR. SinhaS. SethiM. SalmonaA. GeorgeV. BalGeetika SinghA. DindaP. HariS. RathM. Dragon-DureyA. Bagga
ABSTRACTS
Bhatia D, Patino E, Kallinos E, et al. Macrophage-derived cytokines mediate kidney-lung bidirectionally deleterious interorgan crosstalk during kidney fibrosis. J Am Soc Nephrol (Kidney Week-2025).
Bhatia D, Patino E, Kallinos E, Plataki M, Choi AMK, Choi M. Mitochondrial Fusion Protein-mediated Interaction Between Lung Macrophages And Type 2 Alveolar Epithelial Cells Prevents Lung Injury And Deleterious Kidney-lung Crosstalk. Am J Respir Crit Care Med (American Thoracic Society-2025).
Campbell C, Federman HG,….Bhatia D. et al. Myeloid Ferritin Heavy Chain Drives Anemia in CKD by Promoting Iron Sequestration. J Am Soc Nephrol (Kidney Week-2025).
Kallinos E, Torres LK, Bhatia D, Ersoy B, Stout-Delgado H, Choi AMK, Plataki M. Fatty Acid Oxidation Downregulation in Alveolar Epithelial Type 2 Cells Promotes Obesity Associated Acute Lung Injury. Am J Respir Crit Care Med (American Thoracic Society-2024).
Campbell C, Matthews-Balcombe J, Elsayed H, Patino E, Bhatia D, Akchurin O. Iron Sequestration in Young Mice with Chronic Kidney Disease. Pediatric Academic Societies-2024.
Bhatia D, Patino E, Kallinos E, et al. Myeloid and Type 2 Alveolar Epithelial Cell-specific Mitofusins regulate Kidney Fibrosis and associated Lung Injury. Cornell’s Pulmonary Academic Day-2024, WCM.
Federman H, Campbell C, Elsayed H, Bhatia D, et al. Iron Sequestration in Kidney Macrophages Is Essential for Protecting Proximal Tubules from Iron Overload during Iron Therapy in CKD. J Am Soc Nephrol (Kidney Week-2024).
Bhatia D, Patino E, Kallinos E, et al. Mitofusins by Regulating Lung Macrophage-Derived Immune Signals Modulate Monocyte Migration and Interorgan Cross-Talk during Kidney Fibrosis. J Am Soc Nephrol (Kidney Week-2024).
Bhatia D, Plataki M, Choi M. Myeloid and Type II Alveolar Cell-specific Mitofusins Regulate Kidney Fibrosis-associated Lung Injury. Am J Respir Crit Care Med (ATS-2023; Poster Discussion).
Bhatia D, Plataki M, Choi M. Myeloid-specific mitochondrial fusion proteins MFN1 and MFN2 regulate lung injury associated with CKD. J Am Soc Nephrol (Kidney Week-2022).
Patino E, Bhatia D, Vance SZ. et al. Parenteral Iron Therapy Alters Polarization of Kidney Macrophages and Mitigates Kidney Fibrosis in Mice. J Am Soc Nephrol (Kidney Week-2021).
Bhatia D, Capilli A, Nakahira K. et al. Loss of Macrophage MFN 2 but Not MFN1 Suppresses Mitochondrial Biogenesis and Promotes Kidney Fibrosis. J Am Soc Nephrol (Kidney Week-2021).
Bhatia D, Capili A, Nakahira K, et al. Conditional Deletion of Myeloid-specific Mitofusin-2 but not Mitofusin-1 promotes Kidney Fibrosis. J Am Soc Nephrol (Kidney Week-2020).
Bhatia D, Capili A, Nakahira K, et al. Conditional Deletion of Myeloid-specific Mitofusin-2 promotes Kidney Fibrosis. 5th Annual Weill Department of Medicine Research Retreat-2020.
Bhatia D, Capilli A, Nakahira K. et al. Conditional Deletion of Myeloid-Specific Mitofusin 2 Promotes Kidney Fibrosis. J Am Soc Nephrol (Kidney Week-2020).
Patino E, Doty SB, Bhatia D. et al. Analysis of Cortical Bone Transcriptome Reveals Suppression of Bone Formation Pathways by Iron Therapy in Experimental CKD. J Am Soc Nephrol (Kidney Week-2019).
Bhatia D, Chung KP, Nakahira K. et al. Macrophage Mitophagy Deficiency Promotes Experimental and Human Kidney Fibrosis. J Am Soc Nephrol (Kidney Week-2019).
Meza K, Patino E, Dalal V, Bhatia D. et al. Interleukin-6 and anemia in juvenile mice and children with CKD. 51th European Society for Paediatric Nephrology, Annual Meeting-2018.
Akchurin OM, Patino E, Dalal V, Bhatia D. et al. Treatment of Anemia with Oral and Parenteral Iron Leads to Bone Loss in Juvenile Mice with CKD. J Am Soc Nephrol (Kidney Week-2018).
Bhatia D, Chung K.P, Muthukumar T. et al. PINK1MFN2-Parkin-Mediated Mitophagy Dependent Macrophage Reprogramming Protects against Renal Fibrosis. J Am Soc Nephrol (Kidney Week-2018).
Akchurin OM, Patino E, Angara S, Dalal V,
Bhatia D. et al. Dietary Iron Supplementation Leads To Cortical Bone Loss in Juvenile Mice With Adenine-Induced Chronic Kidney Disease. Pediatric Academic Society Annual meeting-2017.
Akchurin OM, Patino E, Bhatia D. et al. Enteral Iron Therapy and Renal Autophagy in Juvenile Mice with Adenine-Induced CKD. J Am Soc Nephrol (Kidney Week-2017).
Bhatia D and Choi ME. Macrophage Mitophagy Modulates Pro-fibrotic response in Renal Fibrosis. J Am Soc Nephrol (Kidney Week-2017).
May C, Bhatia D, Bagga A, Welsh G, et al. Th17 Cells and Podocyte Crosstalk. UK Kidney Week-2017.
Bhatia D, Sinha A, Bagga A. Rituximab modulates T & B cell subsets and urinary CD80 (uCD80) excretion in patients with steroid dependent nephrotic syndrome (SDNS). 17th Congress of the International Pediatric Nephrology Association-2016.
Sinha A, Bajpai J, Saini S, Bhatia D. et al. Serum urokinase type plasminogen activator receptor (suPAR): Marker for renal dysfunction, not for histology. Pediatr Nephrol. Congress of the International Pediatric Nephrology Association-2013.
Sheriff A, Hari P, Thergaonkar RW, Bhatia D. et al. Effect of cholecalciferol supplementation on FGF-23 levels in children with chronic kidney disease (CKD) having vitamin D insufficiency. Pediatric Nephrol. Congress of the International Pediatric Nephrology Association-2014.
Bhatia D, Sinha A, Bagga A. Rituximab modulates T-cells’ but not B-cells’ subsets in patients with steroid dependent nephrotic syndrome (SDNS). XII Asian Congress of Pediatric Nephrology-2014.
Bagga A, Bhatia D. et al. Randomized controlled trial to compare the efficacy & safety of mycophenolate mofetil versus levamisole in children with frequently relapsing and steroid-dependent nephrotic syndrome. Pediatr Nephrol. Congress of the International Pediatric Nephrology Association-2013.
Sinha A., Bhatia D, Hari P. et al. Efficacy and safety of rituximab in difficult to treat Steroid resistant & dependent nephrotic syndrome. The 16th Congress of the International Pediatric Nephrology Association. Pediatr Nephrol. Congress of the International Pediatric Nephrology Association-2013.
Bhatia D, Sinha A, Bagga A. Rituximab increases T-regulatory (Treg) & decreases Th17 lymphocytes in patients with steroid dependent nephrotic syndrome (SDNS). 40th Annual Conference of Indian Immunology Society, Immunocon-2013.
Sinha A, Bhatia D, Gulati A. et al. Efficacy and safety of rituximab in difficult Steroid resistant & dependent nephrotic syndrome. Pediatr Nephrol. Congress of the International Pediatric Nephrology Association-2012.